How Staffing Models in Healthcare Have Changed due to the COVID-19 Crisis
Over the past decade, staffing models in healthcare have most often been designed to balance the value-driven requirements of the Affordable Care Act with a nationwide shortage of medical personnel. At the start of the COVID-19 crisis, staffing models in healthcare underwent significant changes – changes that may be with us for a while.
Nurse scheduling involves advanced planning for a set number of nurses based on historical numbers and anticipated volumes; while nurse staffing rarely looks beyond the next 24 hours to ensure the right number of nurses are in the right place at the right time. Nurse staffing can be complicated by different staffing models in healthcare – of which the three most commonly used are:
- The budget-based model, in which nursing staff are allocated according to a nursing-hours-per-patient-day formula.
- The nurse-to-patient ratio model – which can be mandated by state law universally or for specific units.
- The patient acuity model, in which the needs of patient populations determine each shift’s staffing requirement.
What makes staffing models in healthcare complex is that more than one model can apply at any one time to either a specific department or a healthcare facility as a whole. For example, in Massachusetts, hospitals using the budget-based model are also required by law to have a 1:1 or 1:2 nurse to patient ratio in ICU departments depending on the stability of the patient.
If a major incident occurs – for example a major pandemic – the number of patients being admitted to ICU can increase rapidly. Furthermore, in a post-pandemic scenario, the needs of patient populations can be exacerbated by the short-term non-availability of – or reluctance to attend – non-essential medical procedures during the pandemic. In this scenario, hospitals would have to adopt patient acuity staffing models in healthcare to meet the fluid requirements of patient populations.
The Influence of ACA on Staffing Models in Healthcare
Other than in states where nurse-to-patient ratios are mandated, the biggest influence on staffing models in healthcare is the Affordable Care Act (ACA). Among other provisions, the Act changed the way in which healthcare organizations are remunerated under the Medicare and Medicaid programs so that, rather than being remunerated by volume, organizations are remunerated by the quality of care.
As a consequence, it is now financially beneficial for healthcare organizations to ensure sufficient staff are on duty to minimize the risk of hospital-acquired infections, to provide treatments that reduce readmission, and to support outpatient clinics promoting preventative therapies. Notably, the Act also expands eligibility for Medicare and Medicaid to uninsured patient populations.
The most commonly used staffing models in healthcare mentioned previously evolved as a result of ACA. They tend to be patient-centric rather than department-centric, and tend to focus on the continuum of care rather than a moment in time. However, designing staffing models in healthcare and being able to implement them efficiently do not go hand-in-hand due to the lack of staff availability.
The Underlying Issue with Staffing Models in Healthcare
A lack of staff availability is the underlying issue with staffing models in healthcare. It is a problem that has been increasing in severity for decades and can result in nurse managers wasting several hours a day contacting staff to fill vacant shifts, leaving messages, and then taking callbacks from staff even after the vacancies have been filled.
To best explain the scale of this issue, in 2012 the U.S. Bureau of Labor Statistics published a National Employment Matrix listing the occupations the Bureau anticipated would have the largest increases in job openings over the next ten years. The Bureau then adjusted the projected figure for 2022 to account for industry growth and replacement needs. Job openings in healthcare featured throughout the matrix:
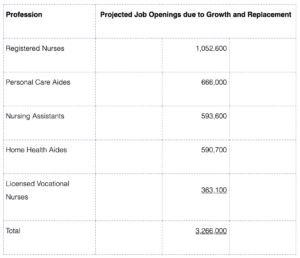
The significant number of projected job openings in the healthcare industry is attributable to a number of factors that includes an aging population, greater accessibility to healthcare, and existing registered nurses reaching retirement age. It is also the case medical and technological advances have resulted in conditions that were once terminal becoming survivable – putting greater pressure on nursing numbers.
However, the industry is failing to train sufficient staff to fill the job openings. According to the latest AACN report on nursing shortages, U.S. nursing schools turned away 80,407 qualified applications from nursing programs in 2019 “due to an insufficient number of faculty, clinical sites, classroom space, clinical preceptors, and budget constraints”. As a result, there is currently a nationwide shortage of 154,018 registered nurses, which is forecast to increase to a shortage of 510,394 nurses by 2030.
Staffing Models in Healthcare during the COVID-19 Crisis
The COVID-19 crisis severely disrupted staffing models in healthcare due to increased patient demand and illnesses among healthcare personnel – exacerbating the lack of staff availability. Most hospitals addressed the increase in patient demand by canceling elective procedures and closing non-essential outpatient clinics, but addressing the lack of staff availability was more complex.
In the worst-hit hospitals, healthcare personnel were repurposed, students were on-boarded, and every available travel nurse was called into action. The problem was that, under these emergency arrangements, previously-used staffing models in healthcare were not appropriate for the circumstances, and many healthcare organizations had to switch to team staffing models.
Team staffing models differ from other staffing models in healthcare inasmuch as nurses with differing levels of skill, education, and qualification work collaboratively as a team. Team members share responsibility for the delivery of patient care, while still maintaining nursing-hours-per-patient-day and nurse-to-patient ratios, despite the model being a significant departure from more familiar models.
While research shows team staffing models in healthcare can improve patient safety and raise staff morale, it can also complicate filling vacant shifts when a team member with a matching level of skill, education, and qualification is required to cover for a sick or vacationing colleague. Unfortunately during the COVID-19 crisis, the majority of vacant shifts were attributable to illness and self-isolation.
Filling Vacant Shifts becomes Further Complicated
As the COVID-19 crisis developed, the complexity of filling vacant shifts increased following guidance issued by the Centers for Disease Control and Prevention (CDC) in July. In order to mitigate staff shortages in healthcare organizations attributable to COVID-19 illnesses and self-isolation, the agency recommended a number of measures including:
- Allowing asymptomatic carriers of COVID-19 to return to work subject to the availability of PPE.
- Allowing mildly symptomatic carriers to return to work – but not in a direct care setting.
- Preventing mildly symptomatic or suspected carriers of COVID-19 from working with colleagues.
- Removing healthcare workers from direct care settings if they display symptoms of COVID-19.
While the recommendations increase the availability of staff, it does create complications when healthcare workers have suspected – but unconfirmed – symptoms and should be self-isolating, when healthcare workers who are allowed to return to work are not allowed to work in direct care settings or with colleagues, or when healthcare workers are removed from health care settings mid-shift.
Furthermore, it was the case – and may still be for months to come – that patients being treated for COVID-19 are transferred to designated healthcare facilities or alternate care sites. In these cases, it is important healthcare workers are told in good time when they are to accompany the patient and continue caring for them in the new venue, or when they are being reassigned elsewhere in the facility.
Finding a Cure for Staffing Shortages in Healthcare
Staffing shortages in healthcare will undoubtedly continue for some time due to the lack of staff availability and continuing staff illnesses. At the same time, patient demand for healthcare will likely increase due to the ongoing COVID-19 crisis, the flu season, and complications caused by the non-availability of – or reluctance to attend – non-essential medical procedures during the pandemic.
Team staffing models in healthcare look like staying for the present, but although they can help address some of the shortcomings of other staffing models, it can be more complicated to fill vacant shifts using this model – resulting in nurse managers wasting more hours a day contacting staff to fill shift vacancies, leaving messages, and then taking callbacks from staff once vacancies have been filled.
Technology cannot resolve the shortage of nurses nor prevent the transmission of COVID-19; but it can help mitigate the complexity of filling vacant shifts in complex staffing environments. Watch this short video below to see how:
It is also worth noting that the issues with staffing models in healthcare are not exclusive to medical staff. While the absence of cleaners, caterers, IT professionals, security personnel, and administrators may not have the same level of criticality as nursing shortages, healthcare organizations still need to fill vacant shifts in these areas to ensure facilities function as best they can during these difficult times.





